KARTAGENER’S SYNDROME (KS)
HIGH RESOLUTION C.T. SCAN OF CHEST (LOW DOSE H.R.C.T.)
Clinical information: Cough & breathing difficulty.
Findings:
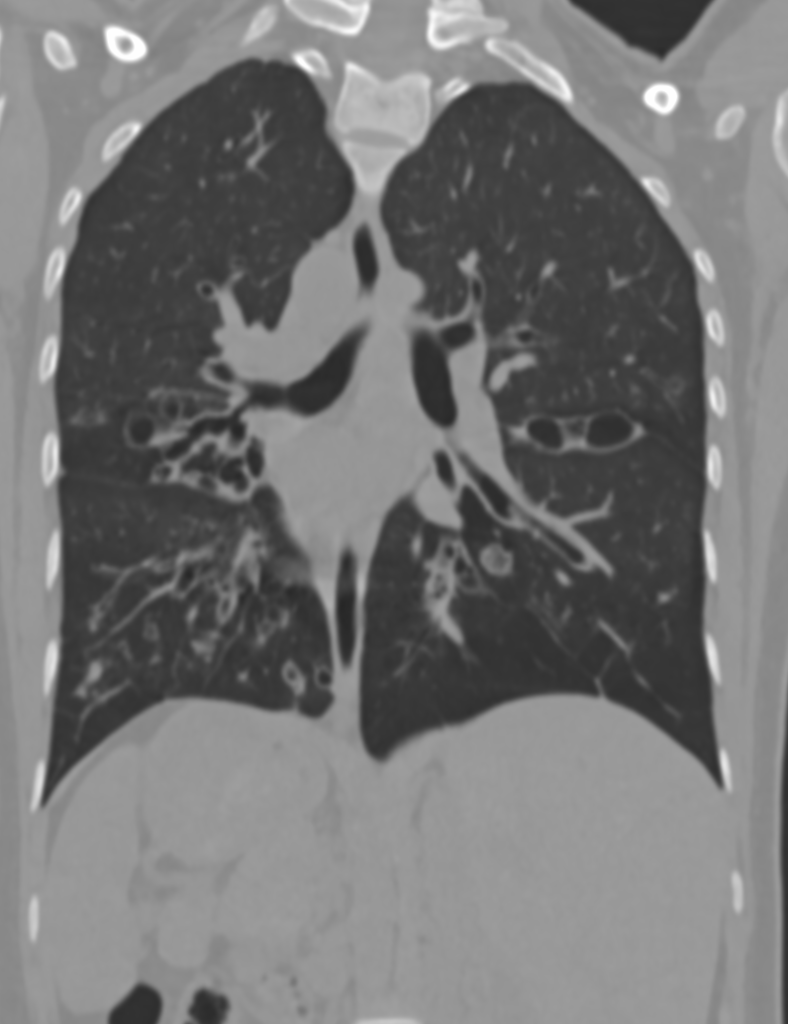
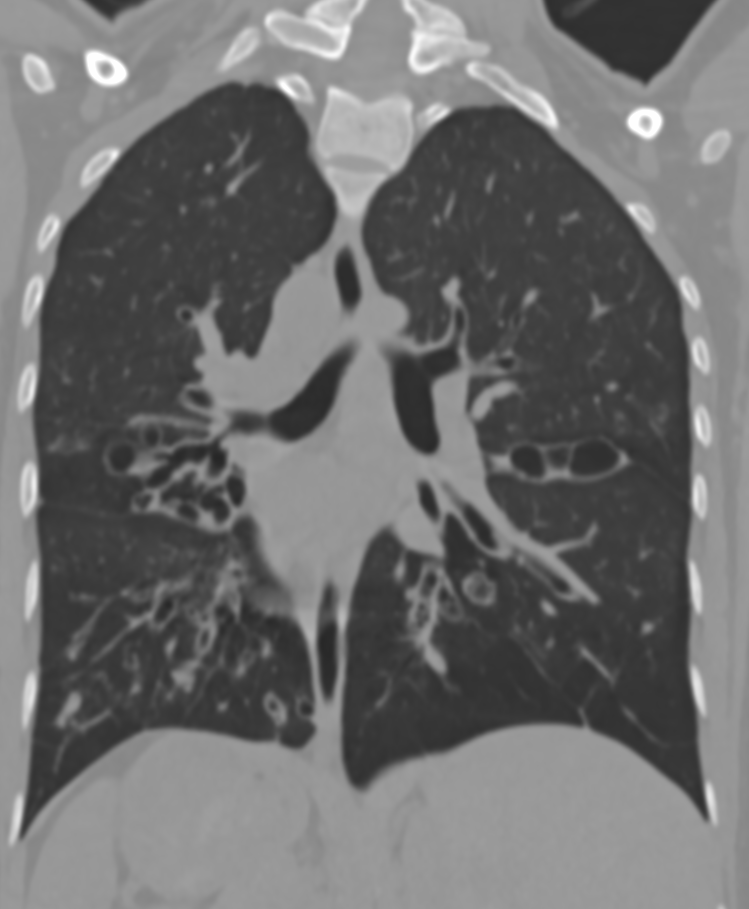
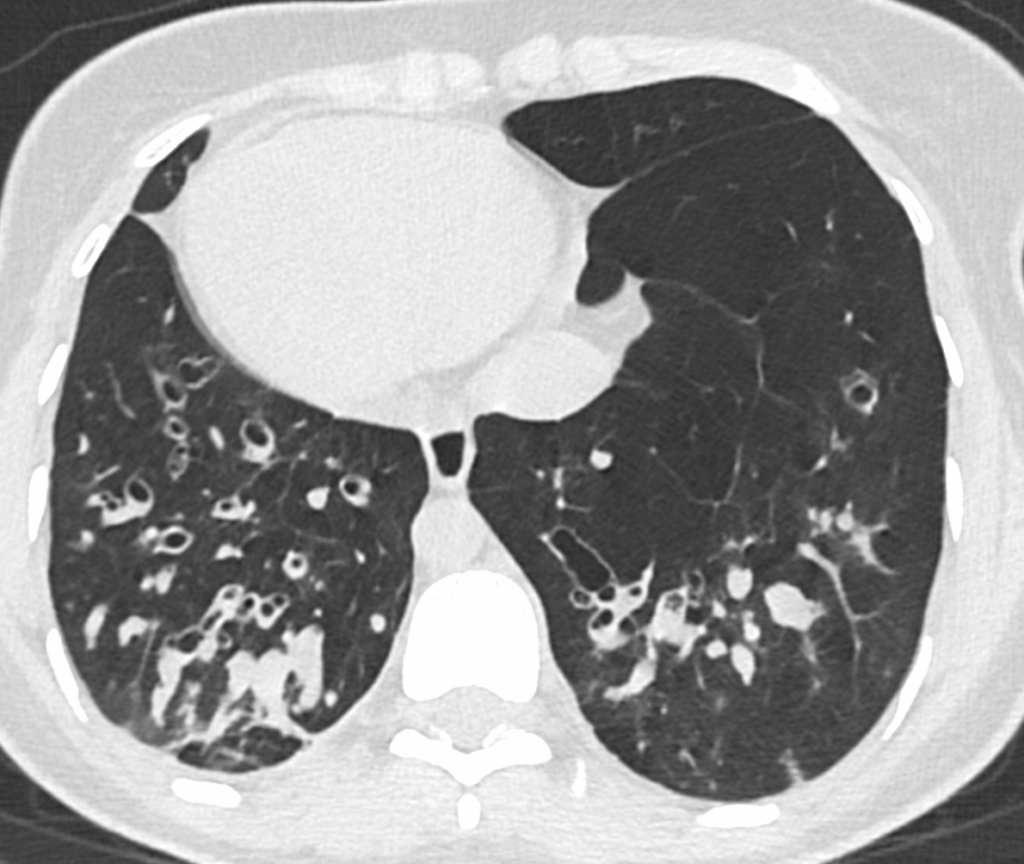
Bronchial wall thickening in both lower lobes. Internal hypodense filling noted in basal segments of both lower lobes.
Multiple tiny nodular opacities noted in both lung fields
Findings suggest possibility of infective etiology – fungal etiology appears likely.
Bronchiectatic changes in both lung fields with collapse and volume loss in right middle lobe and anterior basal segment of left lower lobe as mentioned.
Situs inversus totalis noted with dextrocardia, right sided aortic arch, location of liver in left hypochondrium and spleen and stomach in right hypochondrium.
Discussion:
Respiratory mucosal lining (comprising of nasal cavity, trachea, bilateral mainstem bronchus and intrapulmonary branches of airway) is lined by tiny microscopic ciliary structure that aids in normal mucociliary clearance of secretions.
Any impairment of mucociliary function is due to genetic disorder.
This results in stagnancy of secretions with resultant secondary infection.
One such condition with impaired functioning of ciliary lining of respiratory tract is Kartagener’s syndrome. It is an autosomal recessive congenital disorder.
It is marked by triad of:
- Situs inversus
- Chronic sinusitis
- Bronchiectasis (due to recurrent infection and inflammation of adenoids).
Radiological findings play are crucial role in diagnosis of the syndrome. HRCT of Thorax is particularly helpful.
Findings include:
- Dextrocardia (cardiac apex pointing toward right side), location of stomach and spleen in right hypochondrium and liver in left hypochondrium.
- Changes of sinusitis in the form of mucosal thickening with or without collection in nasal chambers and bilateral paranasal sinuses.
- Bronchiectasis in the form of cystic or cylindrical or varicoid dilatation of airways with internal mucus plugs due to retention of secretions (mucocele).
- Secondary involvement of pulmonary parenchyma in the form of centrilobular nodules, thickening of bronchial wall and peribronchovascular interstitium and development of peribronchovascular consolidations.